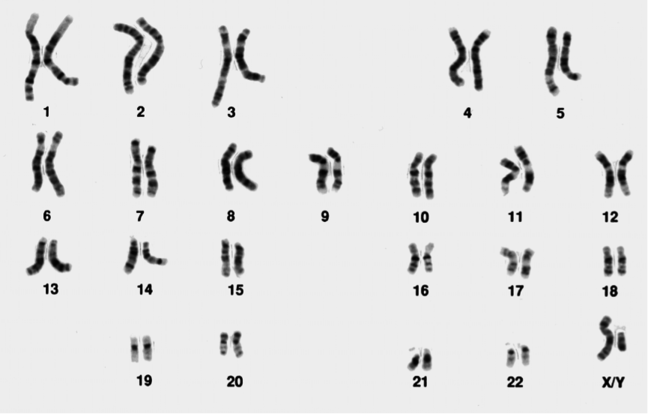
Non-invasive prenatal testing (NIPT) for aneuploidy is rapidly becoming the first line screening test for trisomies 13, 18 and 21 in the first trimester, with more and more hospitals offering the test as part of their routine prenatal care.
Three main methods are used in NIPT. Each is associated with specific advantages and disadvantages and we will discuss each in turn.
Massively Parallel Shotgun Sequencing (MPSS)
This approach was described by Fan et al. in 2008 (PNAS, 1056(16):266-71) and uses next-generation sequencing technologies to generate reads representing chromosome regions across the genome.
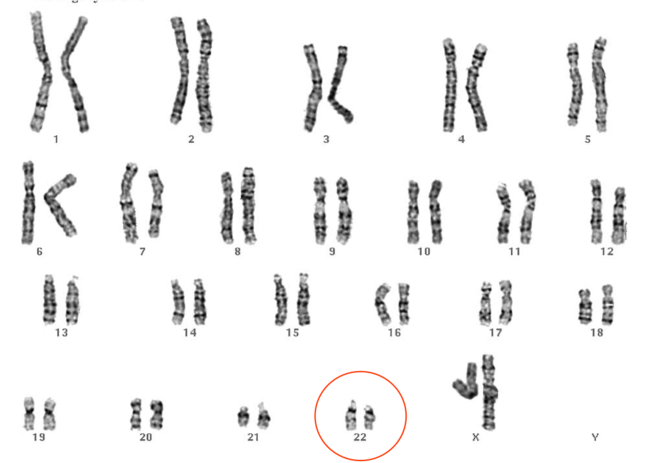
If there is trisomy of a particular chromosome, this would be detectable by a relatively greater number of reads mapping back to that chromosome region on the reference genome. However, this relative increase might be very small indeed.
For instance (as reported by the NIPT diagnostic laboratory at the South West Thames Regional Genetics Service) the reads representing chromosome 21 in a normal pregnancy typically might constitute 1.36% of the total cfDNA (remember, the total cfDNA is maternal and fetal cell free DNA).
However, in a pregnancy affected with trisomy 21, the total contribution of reads mapping to chromosome 21 from both mother and fetus might increase to just 1.42%. That is only a 0.06% difference!
Therefore, to distinguish such small differences in the amount chromosomal DNA found, an incredibly accurate counting and sorting method is required.
A disadvantage of MPSS is that, depending upon the underpinning NGS technology, the method can be costly with only a relatively small proportion of the generated reads being analysed.
Targeted multiple parallel sequencing (MPS)
There are various different forms of targeted MPS. However, they are all underpinned by the same concept - amplifying and quantifying chromosome-specific sequences.
One form of targeted MPS is DANSR (Digital Analysis of Selected Regions). DANSR uses oligonucleotide probes that hybridise to target sequences.
The principle is a bit like that behind MLPA in that it is the probes that are amplified rather than the target sequence. However, in contrast to MLPA, DANSR used three rather than two probes.
The number of each of the amplified probes reflects the amount of target sequence. Therefore, where a trisomy is present, there will be a relatively greater number of amplified oligonucleotides.
An advantage of targeted MPS is that costs are reduced because fewer sequences are generated. However, the targeted sequencing introduces biases and some believe reduces accuracy.
SNP detection
SNP detection is very different from the above two methods as, rather than analysing cfDNA as a whole, it differentiates between maternal and fetal cfDNA. In the commercially available kits, about 20,000 SNPs are utilised.
First of all, the maternal SNP genotype is determined through analysis of the buffy coat (the buffy coat is a layer of blood, mostly containing leukocytes and platelets and therefore not containing cfDNA, obtained through the centrifugation of a whole blood sample).
The plasma is then SNP genotyped which represents both fetal and maternal SNPs. Computationally, the two SNP results are compared and individual fetal and maternal SNP profiles are calculated.
Fetal fraction is first calculated. For instance, if mum is AA and fetus is AB for a given SNP locus, if there is 1000 of AA to 100 AB, then the fetal fraction is 10%.
Then, in order to determine copy number for each interrogated chromosome locus, the maternal and fetal genotypes are compared and evaluated to see whether there is more or less than expected.
Accuracy of NIPT
NIPT has been shown to have high sensitivity and specificity (>99%) for trisomy 21 detection. These figures are currently slightly lower for the other trisomies and for sex chromosome imbalance detection.
It is important to remember that these tests should be considered an advanced screening test rather than a diagnostic test. Sensitivity (likelihood of detecting a trisomy if present) is not the same as positive predictive value (PPV; likelihood of a positive result being a true positive), and the PPV for these tests are rather lower than the sensitivities.
Thus any positive result must be confirmed by invasive testing before any management decisions are made for the pregnancy.
The negative predictive value (NPV; likelihood of a negative result being a true negative) is high for these tests, so in the context of normal ultrasound findings a negative test is reassuring, and confirmation with an invasive test is not usually done.
However, in the context of abnormal findings on ultrasound, a negative NIPT should not be considered reassuring as other underlying chromosomal abnormalities have not been excluded and further invasive testing should be considered.
clinical situations is cell-free fetal DNA analysis not possible for detection of a maternally inherited single gene mutation.
clinical situations is cell-free fetal DNA analysis not possible for detection of a maternally inherited single gene mutation.
NIPD cannot distinguish the presence or absence of a maternally inherited mutation in the fetus. This is because the mother carries the same mutation, so it is present in both the fetal and maternal cell free DNA fractions in the maternal plasma. Researchers are working on developing techniques which analyse the dosage of a given mutation in the maternal blood, but this is technically highly demanding and not currently developed for clinical use.
Twin pregnancy is not likely to cause an inconclusive result when performing NIPT for aneuploidy.
NIPT can be performed in twin pregnancies and is usually informative. If the aneuploidy screening comes back negative then this applies to both fetuses, and in the absence of any other indications, invasive testing can be avoided. If NIPT shows a possible aneuploidy then it could be difficult to know whether one of both foetuses is affected, and invasive testing is indicated.
Twin pregnancy is not likely to cause an inconclusive result when performing NIPT for aneuploidy.
NIPT can be performed in twin pregnancies and is usually informative. If the aneuploidy screening comes back negative then this applies to both fetuses, and in the absence of any other indications, invasive testing can be avoided. If NIPT shows a possible aneuploidy then it could be difficult to know whether one of both foetuses is affected, and invasive testing is indicated.